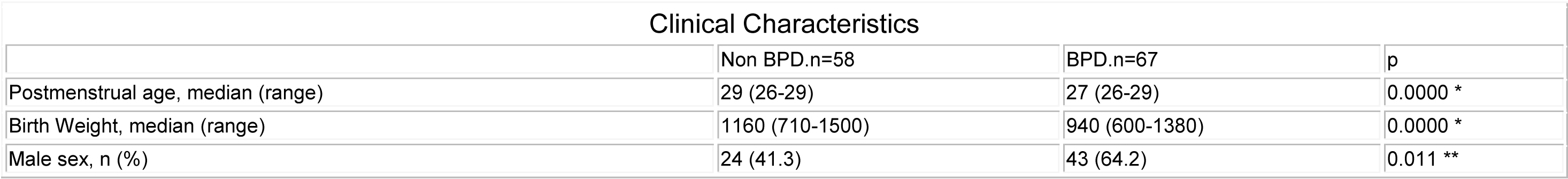
Clinical Characteristics of Patient s Developing Bronchopulmonary Displasia
Gaston P. Perez, Ricardo M. Nieto, Alejandro Dinerstein, Claudio L. Solana, Lidia Otheguy, Miguel Larguia. Neonatologia, Maternidad Sarda, Buenos Aires,Argentina.
BACKGROUND:
25 to 30% of our VLBW infants develop br onchopulmonary displasia (BPD), defined as oxygen requir ement for more than 28 days. Controversies exist about the weight of each one of the clinical variables and n eonatal morbidities described in the literature.
OBJECTIVE:
To evaluate the clinical characteristics of p atients developing BPD compared with a control group without BPD at 40 weeks of postmenstrual age.
DESIGN/METHODS:
Case-control study. Inclusion criteria: in-born infants, postmenstrual age <30 weeks, birth w eight <1500 g and surviving up to 40 weeks of corrected age. Exclusion criteria: major congenital malformations, int rauterine infections or being transferred to other ho spital.
RESULTS:
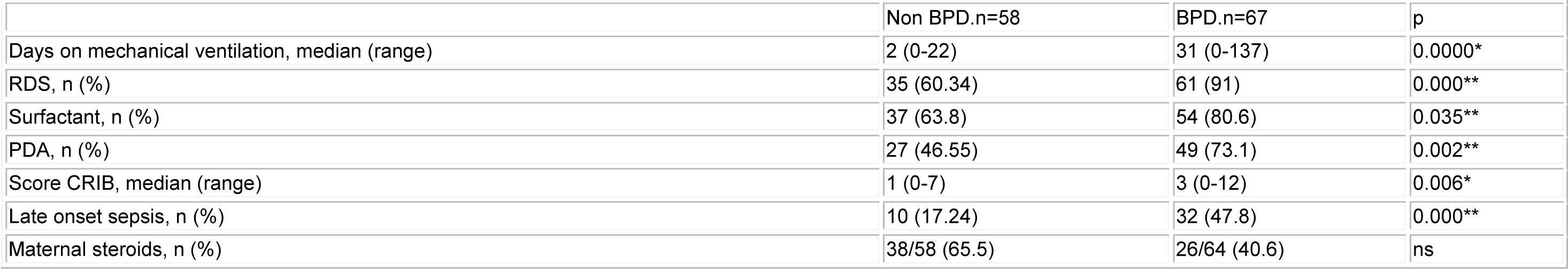
From january 2000 to november 2005, 178 chi ldren were eligible, 52 patients were excluded. 126 patients were evaluated, 67 (53.1%) developed BPD (t able 1-2). By multivariate analysis the following variables were predictive of BPD: male gender (OR: 3,25 CI 95% 1.08 2-9.75), RDS (OR: 5,34 CI 95% 1.37-20.76) and mechan ical ventilation (OR: 42,32 CI 95% 12.93-139.61). The mo del has a good Hosmer-Lemeshow adjustment. It also show s good capacity of classification, with a cut point ≥ 0.25, 80% were correctly classified and a discrimination area under ROC curve of 0.908.
* two sample Wilcoxon test. ** chi2
* two sample Wilcoxon test. ** chi2
CONCLUSIONS:
In our population the predictive variab les for BPD were mechanical ventilation, RDS and male gender. E-PAS2007:618434.7